43F Diabetes on insulin 10 yrs, Hypothyroid 6yrs, HTN bilateral pedal edema 4 months
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's consent. Here we discuss our individual patient's problems through a series of inputs from the available global online community of experts with the aim to solve those patients' clinical problems with the collective current best evidence-based input.
Visit the link below for initial case history:
https://171mkfarhanelogcases.blogspot.com/2023/10/43f-patient-came-to-opd-with-co.html
- ACUTE PULMONARY PEDEMA SECONDARY TO CKD WITH DIABETIC NEPHROPATHY
- HEART FAILURE WITH PRESERVED EJECTION FRACTION(EF56%)
- WITH ANEMIA OF CHRONIC DISEASE
- K/C/O DM2 SINCE 15 YRS
- K/C/O HTN SINCE 10 YRS
- K/C/O HYPOTHYROIDISM SINCE 1YR
- PT WAS BROUGHT TO THE CASUALTY WITH C/O BREATHLESSNESS SINCE 2 DAYS
- HOPI: PT WAS APPARENTLY NORMAL 2 DAYS BACK THEN SHE DEVELOPED BREATHLESSNESS GRADE 2 MMRC INITIALLY AND GRADUALLY PROGRESSED TO GRADE 4 ASSOCIATED WITH COUGH WITH EXPECTORATION - GREENISH MUCOID SPUTUM SINCE 4 DAYS.
- FEVER SINCE 4 DAYS-HIGH GRADE, INTERMITTENT, ASSOCIATED WITH CHILLS AND RIGORS AND RELIEVED BY MEDICATION
- C/O B/L SWELLING OF LOWER LIMBS - PITTING TYPE, EXTENDED UPTO THE KNEE SINCE 1 YR (ON AND OFF)
- C/O DECREASED URINE OUTPUT SINCE 1 YR - VERY MUCH REDUCED SINCE 3 DAYS
- C/O ABDOMINAL DISTENSION SINCE 4-5 MONTHS, ORTHOPNEA PRESENT
- NO C/O CHEST PAIN, PALPITATIONS, PND, SWEATING, GIDDINESS
- K/C/O DM2(SINCE 15 YRS) INITIALLY STARTED INSULIN BUT NOW ON OHAS - SITAGLIPTIN 50 & METFORMIN 1000 & GLIMIPERIDE2
- K/C/O HTN SINCE 10 YRS USING T.PRAZOSIN 5MG
- K/C/O HYPOTHYROIDISM SINCE 1 YR USING T.THYRONORM 150MCG
- K/C/O CKD SINCE 1 YR ON CONSERVATIVE MANAGEMENT
- NOT K/C/O CVA, CAD, TB, EPILEPSY, ASTHMA
- GENERAL EXAMINATION-PT IS C/C/C
- PALLOR, EDEMA PRESENT(PITTING TYPE), NO ICTERUS CYANOSIS LYMPHADENOPATHY
- BP-240/100MMHG
- PR112BPM RR42CPM
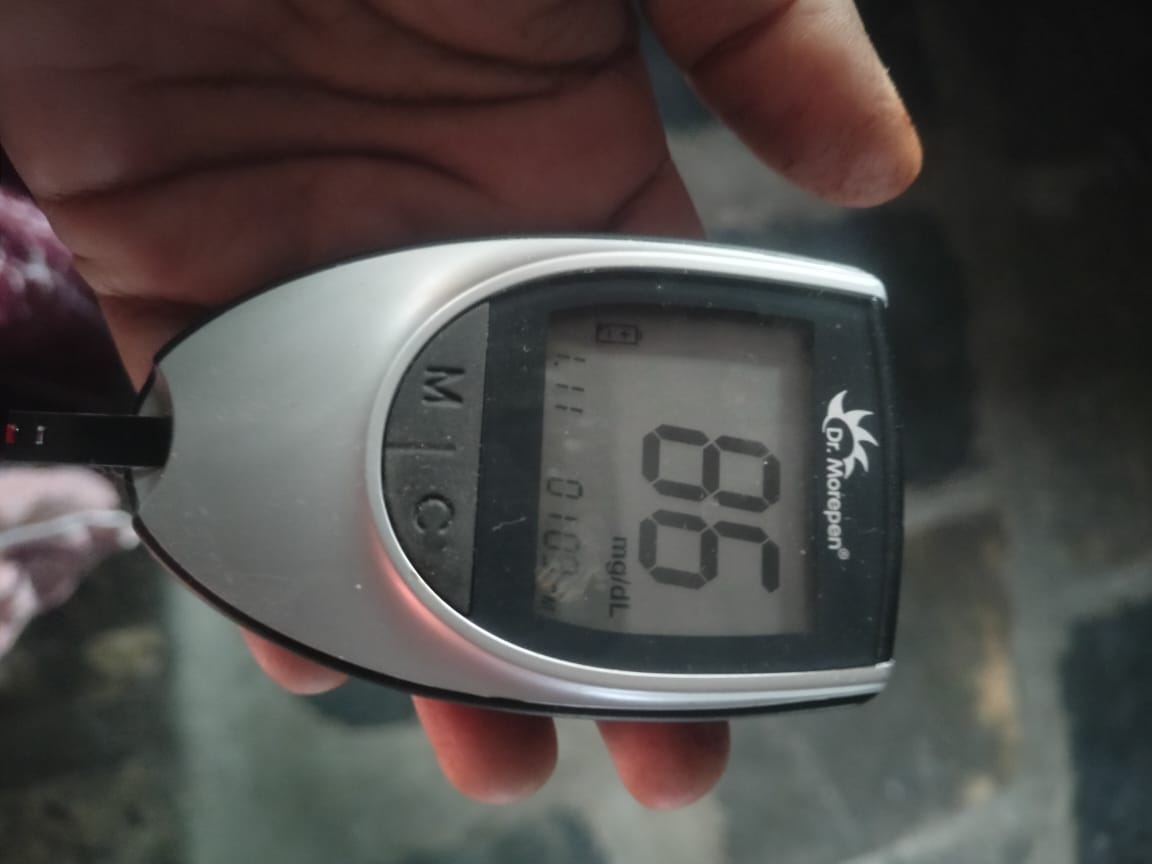
- SPO2 67% AT RA GRBS 100MG%
- SYSTEMIC EXAMINATION
- CVS: INSPECTION-JVP NOT RAISED, CHEST WALL SHAPE NORMAL AND SYMMETRICAL, NO DILATED VEINS/SCARS, KYPHOSCOLIOSIS ABSENT
- PALPATION - APICAL IMPULSE NORMAL NO PARASTERNAL HEAVE, NO THRILLS PERCUSSION - DULL NOTE PRESENT
- AUSCULTATION-S1S2 PRESENT, NO MURMURS
- RESPIRATORY SYSTEM: BAE PRESENT, NVBS, DIFFUSE CREBS PRESENT P/A: SOFT, NON TENDER, NO ORGANOMEGALY
- CNS: NO FOCAL NEUROLOGICAL DEFICITS
Arterial Blood Gas (ABG):
- pH: 7.38
- PCO₂: 32.2
- PO₂: 158
- HCO₃: 19.0
- St. HCO₃: 20.3
- BEB: -5.0
- BEecf: -5.1
- TCO₂: 41.3
- O₂ Sat: 99.3
- O₂ Count: 9.5
Kidney Function Tests:
- Blood Urea:
- First Test: 70 mg/dL (Reference: 12-42 mg/dL)
- Second Test: 88 mg/dL
- Serum Creatinine:
- First Test: 1.9 mg/dL (Reference: 0.6-1.1 mg/dL)
- Second Test: 1: 2.0 mg/dL
- Third Test: 2: 1.5 mg/dL
Serum Electrolytes (Na, K, Cl):
First Test:
- Sodium: 130 mmol/L (Reference: 136-145 mmol/L)
- Potassium: 3.7 mmol/L (Reference: 3.5-5.1 mmol/L)
- Chloride: 101 mmol/L (Reference: 98-107 mmol/L)
Second Test:
- Sodium: 132 mmol/L
- Potassium: 3.5 mmol/L
- Chloride: 102 mmol/L
Third Test:
- Sodium: 134 mmol/L
- Potassium: 3.3 mmol/L
- Chloride: 103 mmol/L
Fourth Test:
- Sodium: 135 mmol/L
- Potassium: 3.6 mmol/L
- Chloride: 98 mmol/L
Liver Function Test (LFT):
- Total Bilirubin: 0.60 mg/dL
- Direct Bilirubin: 0.19 mg/dL
- SGOT (AST): 29 IU/L
- SGPT (ALT): 20 IU/L
- Alkaline Phosphatase: 110 IU/L
- Total Proteins: 5.8 gm/dL
- Albumin: 3.0 gm/dL
- A/G Ratio: 1.06
Hepatitis Screening:
- HBsAg (Rapid): Negative
- Anti-HCV Antibodies (Rapid): Non-Reactive
Complete Urine Examination (CUE):
- Color: Pale yellow
- Appearance: Clear
- Reaction: Acidic
- Specific Gravity: 1.010
- Albumin: ++
- Sugar: Nil
- Bile Salts: Nil
- Bile Pigments: Nil
- Pus Cells: 4-6
- Epithelial Cells: 2-3
- Red Blood Cells: Nil
- Crystals: Nil
- Casts: Nil
- Amorphous Deposits: Absent
- Others: Nil
Thyroid Profile:
- T3: 0.36 ng/mL
- T4: 15.17 µg/dL
- TSH: 5.4 µIU/mL
- INTERMITTENT C-PAPFLUID
- RESTRICTION LESS THAN 1LIT/DAY
- SALT RESTRICTION LESS THAN 2-3GMS/DAY
- INJ NTG 1CC IN 4ML NS ICC IV STAT
- INJ.LASIX 40MG IV BD
- INJ.HAI S/C TID ACCORDING TO GRBS
- T.PRAZOSIN 5MG PO/OD
- T.THYROXIN 150MCG PO/OD BEFORE BREAKFAST
- NODOSIS 500MG PO/OD
- T.OLKEN TRIO PO/OD
- INJ.AUGMENTIN 1.2GM IV TID
- SYP ASCORYL LS 10ML PO/TID
- T.VYMADA 50MG PO/BD
- T.VYSOV-D 100/10 PO/OD
Dietary Restrictions:
- Fluid Restriction: Less than 1 lit/day
- Salt Restriction: Less than 2-3 gms/day
Medications:
- Inj HAI S/C: 6 units BD 8 AM and 8 PM before food
- Tab Augmentin 625 mg: PO/BD x 3 days
- Tab Lasix 40 mg: BD x 15 days
- Tab Vysov D 100/10: PO/OD x 15 days (1 PM)
- Tab Vymada 50 mg: PO OD x 15 days
- Tab Prazosin 5 mg: PO OD x 15 days
- Tab Olkem Trio: PO OD x 15 days
- Tab Nodosis 500 mg: PO BD x 15 days
- Tab Thyronorm 150 mcg: PO OD to be continued
- Tab PAN 40 mg: PO OD
- Syp Ascoril LS 10 ml: PO BD x 5 days
- T.Shelcal XT: PO OD at 2 PM for 15 days
- Monitor Glucose At Home: Check using a Glucometer at 7 AM, 10 AM, 4 PM, 10 PM
- Avoid self-medication without doctor's advice.
- Do not miss medications.
For Treatment Inquiries Patient/Attendant Declaration:
admitted with severe heart failure secondary to her
metabolic syn with Diabetes since 12 years
Patient Advocate:
For night
OPD now:

























Comments
Post a Comment