29F Intermittent Chest pain October 2024 Global PaJR
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's consent. Here we discuss our individual patient's problems through a series of inputs from the available global online community of experts with the aim to solve those patients' clinical problems with the collective current best evidence-based input.
Body weight (May 17) = 49Kg
Since the October 2024 begins, patient is suffering from chest pain that is localized in the center spreading to whole chest. Upon every moment or pressure there is extreme pain felt. If the patient is at rest, nothing is felt but upon every moment like getting up from bed while lying down, bending forward to pick up something from the floor, moving hands, sneezing, kneading the dough or washing utensils. Some days it is intense when every little moment have extreme pressure & pain in chest and other days it is less intense but it is sitting there all the time. Same Indian doctor diagnosed it as "Chest pain as Atypical complication of Chronic GERD".
Since childhood
- Archilles tendon
- Severe headache that resides after 3 to 5 days (Currently frequency is less).
Initial Life Phase
- Patient weighted 5 pounds at birth. She was delivered by c-section. Her birth order is third and last.
- Other than the occasional sickness, she used to get sick always during exams and results. She was healthy. She used to eat everything. She had no digestion problem.
- In 2002, she was in 1st standard when she got infected with chicken pox. It took her 1.5 months to recover as they were big in size.
- In 2008, she got sick. Medical tests were done and she was diagnosed with Jaundice. she was advised a complete bed rest and medicines. she was on boiled potatoes mostly. She recovered in 2.5 months.
- Later on she was having recurring fever and throat infection every 2-3 months interval.
Journey from beginning of typhoid to recovery of TB
- In October 2010, she was in 9th standard when her health starts to worsen. She was having extreme pain in abdomen, bloating, vomiting out whatever she was eating followed by high grade fever & shivers. Medical tests were done and she was diagnosed with typhoid. After one month's treatment her condition didn't get better. Tests were repeated and the GP said her typhoid is treated but there was a question mark as to why the high grade fever & digestion issues are not getting better.
- Patient was taken to a pulmonologist. Her multiple tests were done but nothing was found. Only her HB levels were decreasing and her weight. Patient reached to a weight of 45 Kg.
- Patient was having high grade fever of 103/104 degree. Even after giving meds for lowering the fever, the fever gets to its peak of 103/104 degree every 1.5-2 hrs gap. Shivers every time.
- After 4 months, pulmonologist started TB medications on the basis of a case in her family where a member was diagnosed with pulmonary TB a year ago. Doctor indicated that if the condition starts to become better than the TB medications will be continued. (That was a Trial)
- Meds started, a week later she starts to shiver badly, later vomited everything out, trembled badly. Rushed to the emergency and was given painkillers to reside the abdominal pain & to stop the vomiting.
- Pulmonologist ordered a CT scan, in which extra-pulmonary TB was confirmed (Both Lungs + Intestine). TB medications continued.
- Few months later, patient was diagnosed with mumps. She had extremely painful swelled jaw (both sides) and was unable to open the mouth to eat so fluids were given but she was unable to take fluids as well so an injection was given. Later on taking fluids become less painful. It took almost a month to recover.
- After a while her whole body starts to swell from different parts neck, arms, foot, sole. Her doctor lowered the dose of TB meds. Swelling starts to get better but the recurring swelling of the sole took years to subside.
- Her meds were continued for 9months and she was successfully recovered in 2011.
Journey of Post TB complications begins
- Her digestion issues never resolved. Every 2-3 months she was having same episodes.
-Extreme abdominal pain (cramps) that she cannot even walk or move
-Bloating
-Vomiting that when started donot stop
-Pain do not get better with vomiting
-Abdomen feels tight
-No pain killers ever worked
-Rushed to the emergency. They gave combo of pain injections mostly (nospa & voren) and sometimes something in the drip as well. They provide oral meds for a week. With continuing soft diet and meds abdomen feels normal after a week. - Rarely, she had to visit hospital again for another dose of pain injections again after 8-12 hours as the cramps returns with same intensity.
- Her diet was getting restricted & restricted as nobody was able to figure out what food is harming. Sometimes the same food don't harm but the other time it becomes the cause of problem.
- At one similar IBS episode, her pulmonologist ordered abdominal X-ray in that condition and the gas was found in the X-ray.
- In 2014, patient was in 12th standard when she got admitted due to similar condition of pain & vomiting in the hospital for 3 days to keep her under observation by pulmonologist. Surgeon was also involved because they were suspecting intestinal blocks. She was on drip (pain relieving, acid reducing, etc) for 3 days. Multiple tests were done and she was discharged with prescription to follow as nothing severe was found so surgery wasn't performed.
- Occasionally, her neck used to get swelled whenever she slept in the wrong head tilted position.
- Occasionally, she used to get fever of 100 due to tiredness.
- Occasionally, her knees got jammed like locked while sleeping and required a help to straighten it. That was painful.
- These IBS episodes continued with the same frequency until 2016 when she was in her 2nd year of graduation. The frequency reduced and these episodes starts to occur once in 6-7 months.
- In 2nd Year of her graduation her monthly periods cycle reduced to once in 3-4 months. Sometimes periods comes on its own after 3-4 months & sometimes it has to be induced by Duphaston 10mg (Dydrogesterone). In 2017 ultrasound was performed.
After 3-3.5 years it got better when patient was graduated. 1.5 months of naturopathic intervention was also taken.
- Later she was found Vitamin D defficient (level 6). Meds and course of injection was continued. It was back to normal.
- In 2017, her eyesight got weak where distant objects weren't clear and she got a minor number. Doctor said it cannot be reversed. Patient stopped using mobile phone and laptop in the dark for two years. Occasionally wore prescription glasses.
After 3 years her eyesight was back to normal again. - She graduated in Dec 2018. After that frequency of IBS episodes increased more as in once every month.
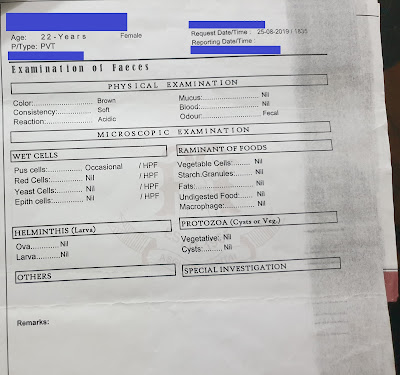
- In August 2019, she got admitted again in the hospital for 3 days by GP. Multiple tests were done and nothing was found. Last day of discharge she got fever so GP delayed the discharge by one more day.
Note: She never used to tell her family in the first hour of the occurrence of pain. After 6-7 hours of extreme pain when she became breathless to bear then she informed.
Psychological Issues with its own physical complications
- Soon after the discharge, patient felt lump in the throat. That lump made it difficult to swallow solid food and drink water. (It subsided after 1.5 years almost)
- She starts to have fire like burning in her abdomen 24*7. (It took 4 years to reduce its intensity to a manageable extent)
- Her whole body feels burning hot.
- Acid reflux started. Happened everyday.
- She can't sleep for as there was discomfort in her abdomen all the time. She can't lye down due to acid reflux.
- She just take a nap in sitting position. (For 1.5 years)
- Her diet was restricted more and she ate only custard, plain rice, wet roti & boiled water. (For 1.5years). Her family thought it will be safest and easily digestible food.
- She was diagnosed with GERD and Functional dyspepsia by her GP.
- Lightheadedness which last for hours so she hang the head off the bedside which made her feel better. One time she fall down due to dizziness & black out. She rested on a bed for a while & she was fine later on.
- Extreme restlessness all the time so she kept walking in the house for hours due to which her feet got corns.
- She can't breathe properly so she sat for hours in front of pedestal fan for comfort but still she had to breath from mouth.
- Flickering of her eyes everyday. Buzzing sound in ear very often.
- Urinary incontinence and rarely poop leaks.
- Pounding heart all the time. She remained scared all the time.
- GP diagnosed her with Anxiety and prescribed anti-anxiety. She took the 1 dose and she kept sleeping for 48 hours. She stopped the medication right away as she donot want to deal with her problem by sleeping.
- She went to another renowned doctor who sent her home by saying it is all her "wehem".
- Her hand trembles all the time.
- Extreme exhaustion & tiredness.
- She had unreasonable pains in her body. Severe chest pain with chest tightening.
- Her eyes become harder to open where it got noticed by a friend who suggested to take therapy but the family declined.
- She felt like the body is shutting down slowly. Her mind was killing her.
- She started taking online therapy from a psychologist secretly from march 2020.
- Her 24*7 severe burning sensation intensity starts to get better after 6 months of its onset and she learned some coping techniques to deal with her anxiety.
- Psychologist recommended to approach a psychiatrist and convinced her to take help of medicine as well because counseling was not enough only.
- After psychiatrist evaluation, co-morbidity of Generalized Anxiety Disorder followed by panic attacks and major Depression was diagnosed.
- Flux 20mg (Fluoxetine HCL) was started once daily and continued for 1 year by psychiatrist. Counseling sessions by psychologist was continued for 6 months.
- She vomited after 4-5 days of taking the medication followed by panic attack.
- 1st episode of her allergy got triggered where she continuously sneezed whole day for a month. She discussed with the psychiatrist where she was told it is not because of medication. Since then time to time she has these allergy episodes up to this date.
- Mood starts to get better with months passed but other than else everything was same.
Journey from 2020 - 2025
- In August 2020, occurring of the IBS episode leads to approaching a gastroenterologist. Who performed some medical tests and declared once and for all "we do not have her cure. Her psychiatric medications will be continued as her treatment is there. She might have to take psychiatric medications & pain killers for her IBS episode for lifetime."
- Patient felt relieved after knowing that truth at that time as every other doctor was just stuck in performing medical tests and providing multiple medications. She was just fed up of it.
- Later that year she got in contact with the doctor from India who after listening to her whole history provided the insight that the patient's bowel movement is slow, it is not regular as emptying a bowel in her case took minimum 3 days. He educated her regarding her issues, gave bowel movement training, tracked her daily routine, asked her to follow low FODMAP diet for few months, did a course of omeprazole and asked her to take only one medicine (omeprazole) whenever any problem arises.
- She starts to eat better, her condition started to improve. With good nutrition she gained weight after more than a decade. From her average weight of 48 she reached to 56 and even 58 with time.
- Since 2021 - 2024, IBS pain episodes were reduced to 2-3 times yearly which was managed by omeprazole only & later Bascopan plus.
- In between these years there is a vitamin D deficiency again, irregularities in periods but it is currently good now. Extreme whole back pain for 6-7 months where patient can't get up from bed and daily functionality was hindered badly. The pain subsided on its own after 6-7 months.
- Since December 2023, patient has a floater in left eye.
- In August 2024, Patient suffered from extreme pain in the eyes followed by Hardness and severe pain in both eyes, Eye movement was painful, Extreme pain in eyelids on touch, Redness, Extreme pain in light (Darkness was soothing) so patient wore sunglasses all the time. Patient took an expert opinion online who prescribed an eye drop ofloxacin. Took it for a week but nothing improved. After 10 days patient took paracetamol and 90% of the problem was resolved within 15 mins. Patient went to ophthalmologist. Her eyesight got checked which was normal. Eyes were evaluated and nothing was found. Doctor ruled out everything major and said mild inflammation is there only. He said those severe symptoms could be due to depression but no reason is certain.
- Since the October 2024 begins, patient is suffering from chest pain that is localized in the center spreading to whole chest. Upon every moment or pressure there is extreme pain felt. If the patient is at rest, nothing is felt but upon every moment like getting up from bed while lying down, bending forward to pick up something from the floor, moving hands, sneezing, kneading the dough or washing utensils. Some days it is intense when every little moment have extreme pressure & pain in chest and other days it is less intense but it is sitting there all the time. Same Indian doctor diagnosed it as "Chest pain as Atypical complication of Chronic GERD".
- Since last 3 Januaries patient is having severe throat infection that takes a month to recover but this January 2025 she had a change of smell as well where everything smells so badly that it was unbearable. After 3 days she got her 70% smell back. After 15 days she got 99% smell back. After a month she got 100% smell back.
- In February 2025, due to constipation she strained a lot for the bowel movement at 10 pm. After 5 hours when she went to pee at 3 am she bled a spoonful of blood from rectum area. She got fever in the morning and then in the evening. She kept in check for the blood for few days but there was no sign just pain in the area. She also had pain in the body since few days due to physical work load which was the reason for the fever probably. Paracetamol helped a lot in this case.
- Later on time to time she had fever either after taking shower or after getting tired. This event happened approx 3 times.
- In march 2025, she slept on hand by mistake for 30 min. After waking up her whole index finger got numb. In 10 mins half of the sensation came back. Remaining half was not intact. Her motor function was normal. Finger looked fine but slightly swollen & heavy. She felt current sensation on touching dorsal side of hand between index finger and thumb. She felt minor unusual sensation till her elbow. Later reduced sensation in half of her middle finger also just like index finger. While giving it rest, fingers were becoming stiff. So she kept using it and did work with it. Now it is a lot better. Only minor issue is left. This radial pinched nerve issue in right hand comes and go since years.
- At the end of march she again had throat infection. 3 days of antibiotics course was done.
- On 10 March 2025, After eating 1 Guava (without seeds) in empty stomach the IBS pain triggered and with 3 doses of buscopan plus & omeprazole the pain didn't reside. After 4 years it becomes severe that the patient went to the hospital where nospa forte injection was given with a prescription to follow for 3 days.
29 April 2025
PaJR PHR Moderator: The narrative event data below is suggestive of musculoskeletal pain👇
"Upon every moment or pressure there is extreme pain felt. If the patient is at rest, nothing is felt but upon every moment like getting up from bed while lying down, bending forward to pick up something from the floor, moving hands, sneezing, kneading the dough or washing utensils."
29F IBS: Sir what will you suggest about this ?
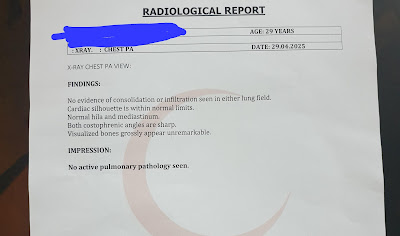
PaJR PHR Moderator: If it's truly musculoskeletal then one need not worry. A chest X-ray image could tell us further.
Also I guess the important radiology images supporting the diagnosis of extra pulmonary tuberculosis in this patient is not available anywhere now?
29F IBS: Ok sir I will go for chest x-ray.
No sir those images are not available now.
Sir what should i do further?
PaJR PHR Moderator: A proper small bowel enema if that is available?
Not that the organic diagnosis will change management at this point of time. I have a patient unpajred but in touch through pm who has exactly similar history and I'm following her up since 2005!
29F IBS: Sir this is small bowel enema, the same you mentioned?
30 April 2025
29F IBS:
1 May 2025
PaJR PHR Moderator: Thanks! The lungs look hyperinflated. Did she ever have any history of bronchial asthma?
29F IBS: No sir. No history of bronchial asthma.
When she was going through mental health issues in 2019. She had severe breathing issues. She used to breath though mouth. Later with years it got better.
In 2020 allergy got triggered she sneezed non stop for a month. Till this date with perfume, dust, smoke or any unknown things triggered the allergy every week where she either get better on its own within an hour or she has to take cetrizine/levocetrizine.
Still with just few physical work or stressed she has breathlessness.
PaJR PHR Moderator: These symptoms are matching her chest X-ray
29F IBS: Sir what is the reason and what is your diagnosis? What you will suggest or conclude?
PaJR PHR Moderator: When was her last attack of breathlessness?
Please describe that in hourly detail
29F IBS: 2 days back on 29 april
12pm
I woke up after 3 hours of sleep.
1pm
I had my 1st meal which i took 1 hour to finish.
2pm - 4pm
After namaz, I searched about musculoskeletal pain and took a nap in between.
4:30pm - 6pm
I pressed my clothes. Got ready and father took me to hospital which is at a distance of 2mins drive.
I was little worried about it so very minor breathing difficulty started.
While i was waiting for my turn in the hospital breathing difficulty started more probably due to anxiousness.
6pm
I came home and went straight to shower.
6:30pm
I prayed namaz which took me 10mins. After that I had call with my sister where talking becomes difficult. Where she said to me to stop talking due to breathlessness. I said it is normal, it happens all the time so i kept speaking and sat down for a while. I went to kitchen and fried kababs.
At 7pm
I prayed namaz
I had my second meal.
7:30pm-9:30pm
I was sitting, resting and talking to mother when breathlessness went away i guess.
9:30pm
I prayed namaz. It took me 20mins.
10pm-12am
I watched a documentary.
12am
I was tired and slept early. Took 1 omeprazole before sleep as there was burning in the abdomen. Woke up in the the middle due to acid reflux, drank some water and slept again in inclined position.
29F IBS: Only little work makes her breathe through mouth and bone/body pains. So whatever physical work she does, she do it with gaps, sit for a while and start doing again.
Talking longer also makes breathing difficult.
PaJR PHR Moderator: Thanks. These details are making things more clearer. I hope it's all being archived in a case report for later recall?
29F IBS: Yes sir I will update it.
3 May 2025
29F IBS: @PaJR PHR Moderator sir what should i do further for this musculoskeletal pain and hyperinflated lungs?
PaJR PHR Moderator: Exercises like yoga including breathing may help
29F IBS: Ok sir thank you












































Comments
Post a Comment